The 5Ps of Counselling
Info: 8013 words (32 pages) Study Guides
Published: 24 Mar 2025
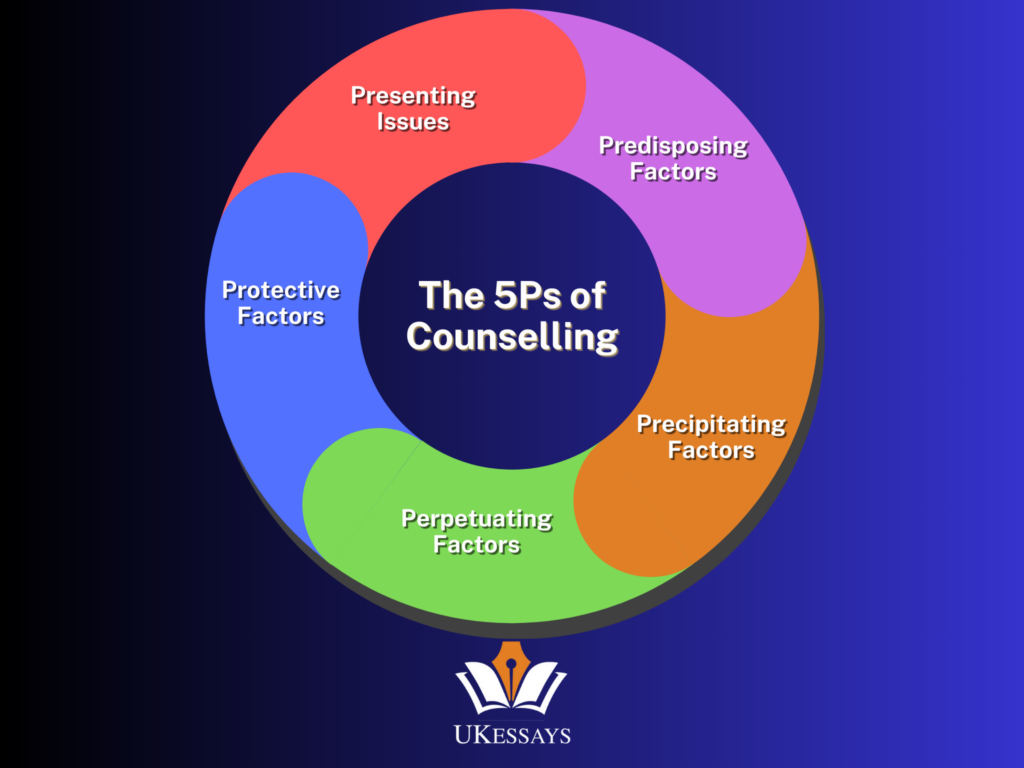
The 5Ps of counselling refer to five key domains that therapists examine when understanding a client’s difficulties. They are as follows: Presenting Issues, Predisposing Factors, Precipitating Factors, Perpetuating Factors, and Protective Factors.
These are the building blocks of a psychological formulation, which is a structured summary of a person’s problems and the factors contributing to them. Formulation using the 5Ps is an alternative or complement to a medical diagnosis. Namely, it explains a client’s issues rather than just labelling them (Macneil et al., 2012). The 5Ps model is widely used because it provides a holistic, systematic framework to organise complex information about a client’s life into a coherent narrative (Johnstone and Dallos, 2014). This approach is idiographic, meaning it is tailored to the individual. In turn, it helps in understanding mental health problems in their context rather than a one-size-fits-all category (British Psychological Society, 2011).
lBy considering the 5Ps, counsellors can identify what problems a person is facing. They can also identify why those problems have developed and what keeps them going.
In sum, the 5Ps of counselling are crucial for formulating a detailed picture of a client’s mental health. They guide effective intervention and collaborative understanding between the client and therapist (NICE, 2014).
What is Formulation in Psychology?
In professional practice, formulation is the process of making sense of a person’s psychological difficulties by drawing together the various influences and factors in their life into an explanatory framework. Unlike a diagnosis which simply names a set of symptoms, a psychological formulation is a working hypothesis about the causes and maintaining factors of an individual’s problems (bMindful Psychology, 2023).
It is often described as telling the “story” of the person’s problems. It links past events, current circumstances, and personal strengths to the development of their mental health issues (Johnstone and Dallos, 2014). Formulation plays a central role in counselling and psychotherapy because it guides the choice of interventions and tailors treatment to the individual (Macneil et al., 2012).
For example, the UK’s National Institute for Health and Care Excellence (NICE) emphasises that formulation provides an explanation of why a problem has occurred and what is maintaining it, and it should inform the therapy plan (NICE, 2014). Formulation is typically a collaborative process. The counsellor and client work together to agree on how the problems can be understood, using language the client finds relatable (BPS, 2011). Importantly, a formulation is not fixed – it’s a dynamic hypothesis that can be revised as new information emerges (Persons, 1989). The 5Ps formulation model has become one of the most popular frameworks for case formulation in psychology. This is because it ensures that the formulation covers multiple relevant domains (predisposing, precipitating, etc.) in a structured way.
In summary, formulation in psychology is about understanding mental health issues in-depth, beyond symptoms. It does this by mapping out all the influencing factors (cause, trigger, maintenance, and strengths) to plan more effective support.
Breaking Down the 5Ps
The 5Ps framework breaks a case formulation into five areas. Each “P” represents a category of factors to consider when understanding a client’s mental health story. We will explain each of the 5Ps in turn – Presenting Issues, Predisposing Factors, Precipitating Factors, Perpetuating Factors, and Protective Factors – including their meaning, significance, and examples of each. By examining all five, therapists ensure a comprehensive formulation that address:
- What is happening;
- Why it might have happened;
- What set it off;
- What keeps it going, and;
- Ultimately, what could help.
Presenting Issues
Presenting issues (or “presenting problems”) are the problems that the client reports or shows up with in counselling. In other words, this category defines what brings the person to therapy – the symptoms, emotions, or difficulties they are currently experiencing and want help with. It goes beyond a diagnostic label by detailing how the person’s life is affected (Macneil et al., 2012).
For example, a client might present with “persistent low mood, loss of interest in activities, and frequent tearfulness” rather than just “depression.” Identifying the presenting issues is important because it clarifies the focus of therapy from the outset and ensures therapist and client have a shared understanding of the problems (Johnstone and Dallos, 2014).
It also helps in setting goals – by specifying the issues, one can determine what needs to change for the client to feel improvement. Presenting issues typically include the client’s thoughts, feelings, and behaviours that are problematic (bMindful Psychology, 2023). They can be external problems (e.g. conflict at work, social withdrawal) or internal experiences (e.g. anxiety, hallucinations).
Examples of Presenting Issues:
- Ongoing feelings of anxiety in social situations lead to avoidance of gatherings.
- Episodes of low mood and hopelessness that interfere with daily functioning.
- Difficulty controlling anger, resulting in frequent arguments with family.
- Intrusive traumatic memories causing nightmares and poor sleep.
These examples illustrate how presenting issues are described in concrete terms. Pinpointing the presenting issues answers the question: “What are the key problems right now?” This is the first step in a 5Ps formulation.
Predisposing Factors
Predisposing factors are the historical or longstanding factors that increase a person’s vulnerability to developing mental health problems. In other words, these are factors in the person’s background that predisposed or set the stage for the presenting issues. Predisposing factors can be biological, psychological, or social in nature (Macneil et al., 2012).
For instance, a family history of mental illness might indicate a genetic predisposition to conditions like depression or anxiety. Similarly, certain personality traits or early life experiences (like childhood trauma) can leave someone more susceptible to difficulties later on. In the context of mental health, predisposing factors mean those factors that have been present for a long time (often years or decades before the current problem) and have laid the groundwork for the issue. They do not cause the problem on their own, but they create a vulnerability (Kuyken et al., 2009). Understanding predisposing factors in mental health is significant because it highlights why this person might be struggling in this way. It provides insight into the person’s life story and background.
For example, someone who experienced neglect as a child may have developed core beliefs of low self-worth, which predispose them to depression when facing losses in adulthood. counsellors consider these factors to ensure the formulation is not just about immediate triggers but also deeper roots of the problem. As one formulation guide notes, predisposing factors can include things like early attachments, past trauma, chronic medical conditions, or longstanding beliefs that made the individual vulnerable.
By identifying predispositions, therapists can address long-term issues (such as unresolved past events or ingrained thought patterns) as part of the therapeutic work.
Examples of Predisposing Factors (Mental Health)
- Early life trauma – e.g. abuse or bullying in childhood leading to vulnerability to later anxiety or trust issues.
- Family history of mental illness – e.g. a parent with depression (genetic and environmental risk for the child’s own depression).
- Chronic health problems or disability during formative years – which might affect self-esteem or stress tolerance.
- Long-term personality traits or beliefs – e.g. perfectionistic personality or low self-esteem established since adolescence.
- Social disadvantage or isolation in upbringing – e.g. prolonged childhood poverty or social isolation affecting development of coping skills.
These predisposing factors help explain why the person might have been likely to develop the presenting issues. They set the stage upon which more immediate triggers can act. Not everyone with a given predisposition will develop problems, but these factors increase the risk.
Precipitating Factors
Precipitating factors are the triggers or events that directly sparked the current problems. In plain terms, they answer the question: “Why now?” – what has happened recently to precipitate (bring on) the presenting issues. If we ask what precipitating factors mean, it refers to the specific stressors or changes that occurred proximate to the onset of the difficulties. These can be one-off events or a chain of events, and they often interact with the person’s vulnerabilities. Common precipitating factors include acute stresses like losses, conflicts, or changes. For example, the death of a loved one, the breakdown of a relationship, losing a job, a sudden illness, or any significant negative life event can act as a precipitant for mental distress.
Sometimes positive events can also precipitate stress (e.g. a job promotion might trigger anxiety due to pressure). Precipitating factors can also be internal, such as a sudden physiological change (like hormonal shifts) or starting to use a new substance, which then triggers psychological symptoms. Identifying precipitating factors is crucial because it highlights the catalyst for the current episode of difficulties (Macneil et al., 2012). It gives context to why the person’s mental health issue has flared up at this point in time.
Moreover, these factors are often key targets for intervention. For instance, if a traumatic event precipitated PTSD symptoms, therapy will likely address that trauma. Understanding precipitating causes also helps validate the client’s experience. You can, for instance, adequately respond “Given what happened to you recently, it makes sense you’re struggling now.” It’s important to note that precipitating factors often work together with predisposing factors. In essence, a person with vulnerabilities might cope fine until a significant stressor occurs, precipitating the crisis.
Examples of Precipitating Factors:
- Job loss or school failure – e.g. being laid off from work. This then triggers a depressive episode in someone already prone to depression.
- Relationship breakdown – e.g. a painful breakup or divorce precipitating intense anxiety or substance misuse.
- Bereavement – e.g. the death of a family member leading to acute grief, depression, or relapse of a prior condition.
- Acute conflict or trauma – e.g. experiencing an assault or a major argument in the weeks before onset of symptoms.
- Onset of a health problem – e.g. sudden diagnosis of a serious illness precipitating health anxiety or panic attacks.
- Substance use or change in medication – e.g. starting heavy alcohol use or stopping an antidepressant suddenly, which triggers mood instability.
These precipitating factor examples show the kinds of recent events that can push a person into crisis or symptom onset. In formulation, acknowledging precipitating factors (the triggers) ensures we address the immediate causes of the client’s presenting issues (for instance, problem-solving the stressor or processing the trauma). It answers “What set off the problems?” in the 5Ps formulation.
Perpetuating Factors
Perpetuating factors are the factors that maintain the problem over time or make it worse. Even after the initial trigger has occurred, certain patterns can cause the person’s difficulties to continue (to perpetuate). Perpetuating factors are essentially the “keeping it going” elements in the situation. They can be internal (like biological or psychological processes) or external (like ongoing circumstances). For example, in depression, a perpetuating factor might be social withdrawal – the person isolates because they feel low, but that isolation in turn fuels the depression further. In anxiety disorders, avoidance of feared situations is a classic perpetuating factor, because while it relieves anxiety short-term, it prevents the person from learning that the situation might be safe, thus keeping the anxiety cycle going (Clark et al., 2005).
As an example, a therapist might work with a client to replace an unhelpful coping strategy (like drinking to cope with anxiety) with a healthier one, thereby removing a perpetuating factor. Perpetuating factors are sometimes referred to as “maintenance factors” in cognitive-behavioural therapy. This highlights that therapy should focus on what is currently sustaining the disorder (Beck, 1979).
Other perpetuating factors can include ongoing stressors (e.g. an unsupportive home environment, continuing substance abuse, or an unhealthy relationship) that continuously provoke the problem. Biological perpetuating factors are also possible: for instance, in bipolar disorder, irregular sleep patterns can perpetuate mood instability. From a formulation perspective, identifying perpetuating factors is vital because these are often targets for therapeutic change. By altering or removing these maintaining factors, the client can break out of the cycle of their problem (Persons, 1989).
By explicitly listing perpetuating factors in a 5Ps formulation, the counsellor ensures they understand what needs to change to resolve the issue, not just what caused it initially.
Examples of Perpetuating Factors:
- Avoidance or withdrawal behaviours – e.g. a person with social anxiety continues to avoid all social contact (this maintains the anxiety because they never get a chance to disconfirm their fears).
- Maladaptive coping strategies – e.g. an individual copes with stress by binge drinking or self-harm. These behaviours provide temporary relief but ultimately sustain or worsen the underlying problem.
- Ongoing stressors – e.g. staying in a high-conflict relationship or stressful job can perpetuate depression or anxiety because the source of stress is constant.
- Cognitive patterns – e.g. persistent rumination (“overthinking”) or catastrophic thinking can keep a person stuck in a depressed or anxious state (the negative thinking feeds the emotional distress).
- Biological factors – e.g. chronic insomnia perpetuating anxiety or mania; or side effects of medication (like stimulant misuse causing continued psychotic symptoms).
- Lack of treatment adherence – e.g. not taking prescribed medication or not attending therapy sessions. Which allows the problem to continue unchallenged.
These perpetuating factors examples demonstrate how various elements can form vicious circles that maintain psychological difficulties. In the 5Ps model, breaking these vicious cycles is often a primary focus of intervention. By recognising what factors exacerbate the problem, a counsellor can strategise with the client on altering those factors
For instance, gradually confronting avoided situations, or improving sleep hygiene, or resolving a chronic stressor). In summary, perpetuating factors explain why a problem doesn’t just fade away on its own and what needs to be addressed for lasting change.
Protective Factors
Protective factors are the strengths, supports, or resources that help the person maintain or regain mental well-being in the face of difficulties. They are essentially the positive side of the formulation – the factors that protect against the worsening of the problem or that foster resilience. Protective factors can be internal (personal strengths, skills, coping strategies, values) or external (social support, community resources, stable job, etc.). Including protective factors is a crucial part of a holistic formulation, as it ensures the focus isn’t only on pathology but also on resilience (Kuyken et al., 2009).
Historically, older models of case formulation sometimes neglected protective factors. But modern approaches emphasise them because building on a client’s existing strengths can significantly improve outcomes (Kuyken et al., 2009; Macneil et al., 2012).
For example, a client might have a supportive family, a hobby they are passionate about, or a strong sense of humour – these can all be protective in helping them cope with stress. By identifying these, the therapist can encourage the client to draw upon them more. Protective factors are also important for instilling hope: when a client and therapist recognise that not everything is “going wrong” and that there are some positives to leverage, it can increase optimism and motivation in therapy (Chadwick et al., 2003).
In the 5Ps framework, protective factors examples might include things like a good social network, prior success in overcoming challenges, religious or spiritual faith, good physical health, or any talent/interest that gives the person joy or confidence. Emphasising protective factors aligns with a strength-based approach to counselling – it reminds us that the client is not defined solely by their problems.
Examples of Protective Factors:
- Strong social support – e.g. close friends or family members who provide emotional help and practical assistance in times of crisis.
- Engagement in meaningful activities – e.g. hobbies like art, sport, or music that give the person a sense of accomplishment. They can also be a distraction from problems.
- Personal strengths or skills – e.g. a good sense of humour, creativity, intelligence, or problem-solving skills that help in coping with adversity.
- Previous coping success – e.g. having overcome difficulties in the past, which provides confidence and learned coping strategies for current issues.
- Access to support services – e.g. being in contact with a support group, a mentor, or receiving counselling/therapy already.
- Resilient personality traits – e.g. high optimism, determination, or faith (such as cultural or spiritual beliefs that provide comfort and meaning).
By noting protective factors in a formulation, counsellors and clients can plan how to use and strengthen these positive factors as part of the intervention. For instance, if a client’s protective factor is a supportive grandmother they trust, therapy might involve encouraging them to reach out to her during tough times. Research suggests that including protective factors in formulations is linked to better outcomes. This may be because it boosts resilience and hope (Kuyken et al., 2009).
In practice, this part of the 5Ps helps answer: “What is keeping the person going? What can we build on to help improve things?” It ensures the formulation is balanced, not just a list of problems, but also an appreciation of resources that can aid recovery.
5Ps Formulation in Different Therapeutic Approaches
The 5Ps formulation model is a trans-theoretical framework, meaning it can be applied in various schools of therapy (Weerasekera, 1996). Different therapeutic approaches use case formulation. But they may emphasise different aspects of the 5Ps or conceptualise them through their own theoretical lens. Here we examine how the 5Ps model is used in three approaches: Cognitive-Behavioural Therapy (CBT), Psychodynamic Therapy, and Integrative approaches. Despite differences, the 5Ps provide a common language that can bridge approaches.
Many clinicians find the 5Ps flexible enough to incorporate cognitive-behavioural, psychodynamic, systemic, and biological factors all in one framework (Peters, 2020). In fact, the model was popularised as part of an integrative “multi-perspective” formulation to ensure a comprehensive understanding of clients (Weerasekera, 1996).
Cognitive-Behavioural Therapy (CBT) Perspective
CBT is a therapy approach that focuses on the links between thoughts, feelings, and behaviours. In CBT, case formulation is very important for tailoring the standard treatment protocol to the individual (Persons, 1989). CBT therapists often use the 5Ps formulation to broaden the standard ABC model (Activating event, Beliefs, Consequences) by adding past influences and maintaining factors to the picture.
The presenting issues in CBT are usually defined in terms of specific symptoms and problematic behaviours (e.g. panic attacks, avoidance of driving). CBT pays particular attention to precipitating factors (situations or triggers that activate dysfunctional thoughts and beliefs), and perpetuating factors in the form of cognitive and behavioural maintenance cycles (for example, safety behaviours or unhelpful thinking patterns that keep the anxiety going).
Predisposing factors also receive consideration, such as:
- core beliefs rooted in childhood or;
- any prior learning that makes the person vulnerable to current thinking patterns (Beck, 1979).
However, CBT formulations may focus slightly less on long-term history than, say, psychodynamic ones. They include it, but the emphasis is on how those predispositions are influencing here-and-now cognitions. Protective factors in CBT might be the person’s existing coping skills or support that can be harnessed (Kuyken et al., 2009). In practice, many CBT therapists use a version of the 5Ps called the “CBT case conceptualization” or “five-part model.” This explicitly maps out triggers, thoughts, emotions, behaviours, and physiological responses (a slight variation of 5Ps). But they often still incorporate life history (predisposing) and strengths (protective) into that map.
Alignment with CBT Empiricism
The 5Ps framework aligns well with CBT’s empirical style. You can test or address via therapy each hypothesis factor (e.g. a perpetuating avoidance behaviour). For example, if the formulation shows that avoiding social situations perpetuates anxiety, the CBT plan will include gradual exposure to social situations to break that cycle. Overall, CBT uses the 5Ps as a practical blueprint, focusing on present triggers and maintaining processes. It also acknowledges past influences and strengths to ensure a comprehensive treatment plan (Persons, 1989).
Psychodynamic Therapy Perspective
Psychodynamic therapy (including psychoanalytic approaches) aims to uncover unconscious processes and how early life experiences influence current behaviour. Additonally, psychodynamic clinicians formulate cases. But their formulation is often more narrative, focusing on internal conflicts and relationship patterns. You can use the 5Ps in psychodynamic formulation, though the terminology might differ slightly.
Predisposing Factors
For instance, predisposing factors in a psychodynamic context might highlight early childhood relationships, attachment style, and childhood trauma or loss (very similar to 5Ps’ idea of long-term vulnerability). A psychodynamic therapist might emphasise how these early experiences led to certain unconscious beliefs or defence mechanisms – these would be part of the predisposition and also partly perpetuating factors (longstanding personality dynamics). Precipitating factors in psychodynamic therapy could be current events that reactivate an old emotional wound or conflict.
For example, a rejection by a friend in the present might precipitate a depressive episode by unconsciously reawakening feelings of abandonment from childhood. Psychodynamic formulations often pay a lot of attention to such links between past and present.
Perpetuating Factors
Perpetuating factors in a psychodynamic view might include ongoing use of defence mechanisms (like denial, projection) or maladaptive relationship patterns (for instance, repeatedly entering into controlling relationships might perpetuate a person’s low self-esteem and anxiety). Presenting issues are acknowledged (e.g. the client’s symptoms of anxiety or depression). However, the therapist sees them as expressions of deeper issues.
Protective Factors
Protective factors in psychodynamic therapy might be ego strengths – aspects of the person’s psyche that are healthy. For instance:
- the capacity for insight;
- strong motivation to improve, or;
- a supportive relationship with the therapist (the therapeutic alliance itself can be a protective factor).
While classical psychodynamic approaches did not always explicitly list protective factors, modern relational psychodynamic therapists do take the person’s strengths into account to avoid an overly pathology-focused view.
Thus, psychodynamic therapists can apply the 5Ps model as a structured check that they have considered the key domains. But they will interpret each “P” through psychodynamic theory. For example, where a CBT therapist sees “perpetuating cognitive distortions,” a psychodynamic therapist might see “underlying unconscious conflicts that remain unresolved.” However, both can be slotted into the perpetuating category.
In summary, psychodynamic therapy uses the 5Ps to maintain a broad perspective (including past, triggers, and current patterns). All with a heavy emphasis on how early predispositions and internal conflicts lead to and maintain the presenting issues. The model’s flexibility allows incorporating concepts like transference (possibly a perpetuating interpersonal factor in therapy if it’s reenacting past relationships) within the 5Ps structure.
Integrative and Other Approaches
Integrative approaches explicitly draw on multiple therapeutic models, and the 5Ps formulation is especially well-suited here. The integrative use of 5Ps was championed by Weerasekera (1996), who described a “multiperspective” formulation model. In an integrative formulation, the therapist might use biological explanations, cognitive-behavioural concepts, and psychodynamic insights side by side when filling out the 5Ps. For example, a predisposing factor for a client’s anxiety might include a genetic predisposition (a biological factor) and an attachment insecurity from childhood (a psychodynamic factor). An integrative therapist doesn’t limit themselves to one theoretical lens – the 5Ps acts as a container to hold all relevant factors.
Presenting issues appear both in terms of symptoms and perhaps the person’s own narrative of their problem. Predisposing factors could range from neurological (e.g. ADHD as a child) to familial (e.g. learned behaviours from parents) to societal (e.g. experiences of discrimination) – whatever applies to that individual case. Precipitating factors and perpetuating factors similarly can span various domains: for instance, an integrative formulation of depression might note a precipitating factor of childbirth (biological/hormonal trigger), plus a loss of identity (existential trigger). Perpetuating factors might include ongoing negative thought patterns (from CBT), marital conflict (systemic perspective), and unresolved grief from earlier loss (psychodynamic).
Addressing every possible factor
Because the 5Ps model is systematic and flexible, it provides integrative therapists a way to ensure they don’t overlook any important area. It is holistic, encouraging consideration of the “whole person.” Many integrative counsellors and clinical psychologists use a 5Ps template in team meetings or case consultations. All in order to organise their thoughts and communicate with colleagues from different backgrounds (e.g. psychiatrists, and social workers).
The model’s systematic yet creative style allows them to plug in various strategies at different points (Peters, 2020). For instance, they might decide a behavioural intervention is best for a perpetuating factor. Meanwhile, a trauma-focused intervention is ncessary for a precipitating factor – all informed by the formulation.
Beyond CBT and psychodynamics, other approaches like systemic family therapy also have formulation practices that parallel the 5Ps (they might talk about family strengths as protective factors, or family patterns as perpetuating factors). An integrative 5Ps formulation essentially serves as a bridge between theories. It gives a common framework where different concepts can coexist in explaining the client’s situation. For instance:
- “schemas” from CBT or;
- “internalised objects” from psychodynamic theory.
In doing so, it upholds the uniqueness of the client (idiographic focus). Then, it tailors interventions drawn from any relevant therapy model to those identified factors.
5Ps Formulation Example
To see how the 5Ps come together in practice, let’s look at a 5Ps formulation example. Below is a worked-through case formulation using the 5Ps framework, based on a composite case (adapted from a clinical example in the literature on co-occurring mental health issues and substance use).
Case Study – “Lena”
Lena is a 27-year-old woman who has been experiencing severe depression and self-harming. She recently lost her job after conflicts with co-workers and has since isolated herself at home. She has a history of childhood trauma and fears abandonment in relationships. Here is how a clinician would formulate Lena’s case with the 5Ps:
Presenting Issues
Lena’s current issues include depressed mood, suicidal ideation, and alcohol misuse. Specifically, after losing her job, she:
- became extremely withdrawn;
- stopped engaging in daily activities;
- began drinking two bottles of wine per day, and;
- has been having thoughts of overdosing on her medication.
She also has ongoing interpersonal difficulties, such as conflicts with co-workers and an on-off romantic relationship causing emotional distress. These are the problems that brought her to clinical attention.
Predisposing Factors
Several long-term factors make Lena vulnerable to these problems. She has a family history of mental illness – her father had depression and died by suicide when she was 12 (indicating possible genetic risk and a traumatic loss). She also endured early life trauma, having been sexually assaulted by a neighbor as a child. These adverse childhood experiences likely contributed to her fear of abandonment and difficulty trusting others. Lena grew up with significant loss, which predisposes her to depressive reactions to loss.
Additionally, her personality tends toward anxious attachment and intense relationships. Her psychologist notes that – this could be another predisposing factor stemming from her early experiences. In summary, Lena’s past (trauma, losses, family mental health history) created a background where depression and relationship issues could easily develop.
Precipitating Factors
The immediate trigger for Lena’s current crisis was the loss of her job and the events surrounding it. In the weeks prior, she had conflicts at work and was missing meetings due to oversleeping (likely related to emerging depression). This culminated in her being fired. This job loss was a significant blow that precipitated a depressive spiral. It also seems to have re-triggered her feelings of abandonment and failure (a psychological precipitant).
In response to losing her job, Lena locked herself in her room for days – during that time her depression deepened and she engaged in self-harm (cutting herself). Another precipitating factor was that around the same time, she had increasing conflict with her girlfriend about the future of their relationship, which further exacerbated her fear of abandonment. These acute stressors – losing employment and relationship turmoil – happened concurrently and set off the acute phase of her illness. In short, the precipitating factors answer “Why now?”:
Lena’s depressive episode and self-harm were precipitated by the sudden stress of job loss (and the cascade of hopelessness and increased isolation that followed).
Perpetuating Factors
Several factors are operating to keep Lena’s problems going and could cause them to worsen if not addressed. One perpetuating factor is her increased alcohol use. While drinking wine numbs her feelings temporarily, it likely disrupts her sleep and mood, making her depression and impulse control worse – thus creating a vicious cycle. Another perpetuating factor is social withdrawal: Lena stopped attending therapy appointments and is avoiding contact with friends or leaving her room.
This isolation removes positive experiences and support that could alleviate depression, and it leaves her ruminating on negative thoughts. There are also perpetuating factors with regard to her treatment. For instance, she is on a medication (paroxetine, an antidepressant) but at a possibly sub-therapeutic dose. Plus, she has disengaged from her psychologist and psychiatrist follow-ups. Accordingly, her condition isn’t under monitor or evaluation (which perpetuates the disorder).
Additionally, ongoing relationship stress is perpetuating her distress. She continues to have unresolved disagreements with her partner, which fuel her feelings of worthlessness and abandonment. Lastly, Lena’s own negative thinking (“I’m a failure, everyone will leave me”) acts as a cognitive perpetuating factor. As such, it deepens her depression.
All these elements maintain the cycle. For example:
- Losing her job made her depressed. In turn;
- Depression led her to drink and isolate. As a result;
- Drinking and isolation in turn deepen the depression and so on.
Recognising these perpetuating factors is key to breaking the cycle. For instance, re-engaging her with therapy, reducing alcohol use, and resolving relationship issues are ways to help her improve.
Protective Factors
Even in this difficult case, there are some protective factors that can aid Lena’s recovery.
First, Lena is physically healthy aside from her psychological issues; she has no chronic medical illnesses, which is a positive. With a bachelor’s degree in computer science, Lena’s education background also shows that she has skills and strengths such as intelligence and prior achievement.
In the past, she had engaged with mental health professionals – the fact that she was seeing a psychologist and psychiatrist (even if she lapsed) indicates she has the capacity to seek help and some insight into her problems; this history of engagement is a strength to build on.
A crucial protective factor for Lena is her brother’s support – her younger brother noticed her crisis and brought her to the hospital. This shows that she is not entirely alone and that someone cares about her well-being. This supportive sibling relationship can be a cornerstone in her recovery. He might help encourage her to stick with treatment, for example.
Additionally, Lena used to play hockey and had an interest in physical activity. Resuming such hobbies could be a protective factor, as exercise and social activity can improve mood.
Building Resilience
Lastly, we can consider that Lena’s decision (with her brother’s urging) to come to the hospital is itself a strength. This shows she has not given up and is now in a setting where she can get help. These protective factors – health, education, family support, prior therapy experience, and hobbies – provide a foundation to build resilience.
In formulating a treatment plan, the therapist would aim to amplify these protective elements.
- Involving her brother in aftercare planning;
- Encouraging a gradual return to enjoyable activities;
- Reminding Lena of skills that helped her succeed in the past.
This case formulation example illustrates how the 5Ps create a structured narrative.
- First, we see what Lena’s issues are;
- Additionally, what long-term and recent factors led to them;
- Moreover, what is keeping her stuck, and;
- Finally, the strengths that can help her improve.
A table or diagram could be drawn to visualise these points, and it would guide the clinician in choosing interventions. For example, trauma-focused therapy for childhood abuse, cognitive therapy for negative thinking, engagement of social support, etc.
In clinical practice, we individualise every formulation. However, 5Ps framework is popular in clinics and training settings because it ensures a thorough, multi-dimensional understanding of the client (Comorbidity Guidelines, 2023). Not all cases are as severe as Lena’s. But even for mild-moderate issues, mapping them in 5Ps can clarify the path to change.
Applications in Clinical and Educational Settings
The 5Ps formulation model is common in both clinical practice and educational contexts to support mental well-being. Its versatility and clarity make it a valuable tool for various professionals.
Clinical Practice (Counsellors and Therapists)
Clinicians such as counsellors, clinical psychologists, psychotherapists, and mental health nurses routinely use the 5Ps formulation when developing a treatment plan for clients. By organising information into presenting, predisposing, precipitating, perpetuating, and protective factors, they ensure a comprehensive assessment. In therapy sessions, they might even share a simple 5Ps diagram with the client to educate them about their own case (helping the client see the connections between, say, their past trauma and current coping behaviours).
This collaborative formulation process can enhance the therapeutic alliance and give clients a sense of understanding and hope. In multidisciplinary clinical teams (e.g., in the NHS or hospital settings), the 5Ps provide a common framework so that, for example, a psychiatrist, psychologist, and social worker can all discuss a case using shared terms. Some NHS services have adopted a “five Ps + Plan” format, adding a sixth step of planning interventions, as a standard way to discuss cases (CNTW NHS Foundation Trust, 2018). Overall, in clinical practice, the 5Ps helps practitioners not to overlook important aspects of a case – it prompts them to consider past influences, current triggers, ongoing behaviours, and strengths systematically.
Clinical Supervision and Training
In educational settings for mental health professionals (like training programs for psychologists or counsellors), the 5Ps are taught as a core skill. Trainees learn how to formulate cases using this structure, often practising in role-plays or with case studies. It serves as a pedagogical tool to teach case conceptualisation. Supervisors often ask trainees questions like, “What are the predisposing factors here? What are the protective factors we can build on?” to guide their thinking.
By learning the 5Ps, students develop critical thinking about cases rather than just memorising diagnostic criteria. University courses in clinical psychology in the UK, for instance, emphasise formulation (BPS, 2011), and the 5Ps model is commonly included because of its clarity. The model is also included in many counselling textbooks and workshops. This educational use ensures new therapists adopt a holistic perspective from the start of their careers.
School and Community Settings (Educators and School counsellors)
Beyond clinicians, even educators such as school counsellors or pastoral care teams use a form of the 5Ps when supporting a young person’s mental health. For example, a school counselling team might formulate why a particular student is having behavioural problems:
- Presenting issue (e.g. anger outbursts in class);
- Predisposing (e.g. learning difficulty, or history of trauma);
- Precipitating (e.g. parents’ recent divorce);
- Perpetuating (e.g. attention from peers for bad behaviour, lack of sleep)
- Protective (e.g. the student has one good friend or a talent in sports).
By using this framework, the school can plan appropriate support (like involving a mentor, addressing learning needs, engaging the student’s strengths in sports).
In higher education, university student counselling services also use formulations to support students in difficulty, mapping academic stress, personal history, and supports to decide on interventions (such as study skills workshops plus therapy). Educators in psychology courses similarly use the 5Ps to teach students about understanding mental health from a biopsychosocial perspective. The model’s clear categorisation is helpful in psychoeducation materials as well. For instance, mental health charities or community workshops might introduce the 5Ps to help people make sense of their own experiences in a structured way.
Clinical Case Conferences and Documentation of the 5Ps in Counselling
In mental health services, practitioners often need to document a case formulation in letters or reports (for example, in a referral or a psychological assessment report). The 5Ps provides a convenient outline for writing these formulations in a report that others (including the client, if they read it) can easily follow. Many services have case formulation templates based on the 5Ps that clinicians fill in after an assessment. Likewise, in case conferences or multidisciplinary meetings, the team may explicitly go through each of the Ps to ensure a shared understanding. This application ensures continuity of care – if a client moves between services, the formulation can travel with them as a summary of their story and needs.
Therapeutic Psychoeducation
Some therapists use the 5Ps with clients as a therapeutic exercise. For example, in cognitive-behavioural therapy for PTSD, a therapist might draw a table on a whiteboard with columns for each P and have the client help fill it in with their own factors. This can empower clients, giving them a framework to articulate their experiences. In group therapy or workshops (such as wellness programs), people might be guided to consider their own 5Ps – e.g., “What are some predisposing factors for your anxiety that you can identify? What are the precipitating triggers?” – and then share in a group. This normalises their experience (others often have similar factors) and highlights areas for change.
In summary, the 5Ps formulation model is widely applied by clinicians and educators alike. Clinically, it’s a backbone of case formulation and treatment planning, ensuring each client receivess, well-thought-out care. In educational and training settings, it’s a key teaching tool that helps future practitioners and clients themselves to conceptualise mental health psoblems in a structured, comprehensive manner. Its usage ranges from therapy rooms to classrooms to community health guides, underscoring its value in promoting understanding and support of mental well-being across settings.
Common Misconceptions and Limitations
While the 5Ps formulation model is a powerful tool, it’s important to be aware of common misconceptions and limitations associated with it:
“Formulation vs. Diagnosis” – Not Either/Or
A common misconception is that using a 5Ps formulation replaces the need for a diagnosis. In reality, formulation and diagnosis serve different purposes and are often used together. The formulation provides the individualised story behind the diagnosis, but it doesn’t negate the usefulness of diagnoses for communication or accessing services. Assuming one must choose between them is a false dichotomy; best practice often involves a bit of both (Macneil et al., 2012).
Superficial or Checklist Use
There is a risk that clinicians (especially those newly trained) might treat the 5Ps as a simple checklist and fill in each category with cursory information without truly integrating it. Formulation is meant to be a thoughtful, hypothesis-driven process. If someone just superficially notes one item under each P without understanding the links between them, the value is lost. This “tick-box” approach is a limitation of the user, not the model per se, but it’s a potential pitfall. Good training and supervision are needed to ensure the formulation is coherent and meaningful, not just a form to complete (Chadwick et al., 2003).
Subjectivity and Reliability
Formulations can be somewhat subjective. Two different clinicians might formulate the same case in slightly different ways, depending on their theoretical orientation or what information they notice. Unlike a medical diagnosis which has (in theory) clear criteria, formulation is more open-ended. There are concerns about inter-rater reliability – whether two practitioners would agree on the formulation for a given client.
Research has shown that more experienced clinicians tend to create higher-quality (more accurate and useful) formulations than less experienced ones. This suggests formulation is as much an art as a science. The lack of a “standardised” outcome means one formulation might emphasise one factor that another clinician overlooked. To mitigate this, often multidisciplinary team formulation sessions are held, so that multiple perspectives contribute to one agreed formulation. Still, the inherent complexity of human lives means formulations will vary. This limitation is important to acknowledge – a formulation is a hypothesis, not absolute truth (Butler, 1998), and it may need revising as new evidence comes to light.
Emotional Impact on Client
Discussing and uncovering the 5Ps can at times be overwhelming or upsetting for the client. For example, talking about predisposing factors means talking about past traumas or losses; precipitating factors might involve recent painful events. If not done sensitively, the process might leave the client feeling worse in the short term. Chadwick et al. (2003) found that while many clients felt formulation increased their understanding and hope, some described it as “saddening, upsetting and worrying” to confront all these aspects of their life.
This highlights the need for therapists to proceed at the client’s pace and ensure a strong therapeutic alliance while formulating. It’s a misconception to think formulation is always experienced as immediately positive by clients – the truth is, it can stir difficult emotions. Therapists must provide support and not rush to fill out all “five boxes” if a client is not ready to delve into something.
Cultural and Social Factors Overlooked
Another potential limitation is that a simplistic use of the 5Ps might lead to underemphasising broader cultural, social, or systemic factors. For instance, a clinician might list a client’s predisposing factors as individual events (e.g. “grew up in poverty”) without fully exploring the societal context (e.g. systemic inequality or discrimination) that underlies their experience. Formulation models are only as good as the awareness of the person using them. If the therapist isn’t culturally competent, they might miss how cultural identity or societal oppression factor into the person’s story.
The 5Ps framework can include those (for example, one could list “experiences of racism” as a precipitating or perpetuating factor for a client’s distress), but it needs conscious effort to do so. A limitation of the model could be that it doesn’t explicitly prompt the clinician about cultural factors unless they intentionally fold those into one of the Ps (perhaps Predisposing or Perpetuating). There’s ongoing discussion in the field about making formulations more culturally sensitive and including an extra “P” for Policy or Power factors to account for social context, though the 5Ps is flexible enough if used thoughtfully.
Evidence of Effectiveness
While many clinicians believe formulation (and 5Ps) is helpful, it’s worth noting that empirical evidence linking formulation directly to better outcomes is still developing. There have been relatively few controlled studies. Some research indicates that a good formulation can lead to more targeted treatment and possibly better engagement in therapy (Johnstone & Dallos, 2014), but it’s hard to measure its effect on symptom reduction. A poorly done formulation might not help at all. Thus, one limitation is that we assume it’s beneficial because of clinical wisdom and patient feedback, but we don’t yet have robust data to quantify how much it improves therapy outcomes. This has led to some criticism that formulation is an unproven “art”. Nonetheless, it’s considered best practice by professional bodies (BPS, 2011) due to its face validity and the consensus that it enhances quality of care.
Excluding the Client’s Perspective
A misconception some practitioners have is thinking the formulation is purely a clinical exercise done by experts. If the formulation is made without the client’s input, it can end up being incorrect or not accepted by the client. For example, a therapist might assume a certain event was precipitating the issue, but the client feels something else was the real trigger. Or the therapist might identify a protective factor that the client doesn’t actually experience as helpful. So, a limitation occurs if there’s lack of collaboration: the formulation might become the therapist’s story about the client rather than with the client.
Modern guidelines stress that the client’s own understanding and goals should be central (BPS, 2011). The client should ideally see the formulation and agree that it “rings true.” Without that, the formulation might not be useful or could even alienate the client (if they feel pathologised or misunderstood). In summary, an unshared or therapist-centric formulation is a common pitfall.
By being mindful of these misconceptions and limitations, practitioners can use the 5Ps model more effectively. This means treating formulations as living hypotheses (open to change), involving the client, being culturally aware, and using the model flexibly rather than rigidly. When used with skill and care, the 5Ps remain a very useful framework despite these challenges. It’s not a flawless tool, but its limitations can be managed with reflective and ethical practice.
Conclusion
The 5Ps of counselling – Presenting Issues, Predisposing Factors, Precipitating Factors, Perpetuating Factors, and Protective Factors – form an essential framework for understanding mental health difficulties and planning effective interventions. In this guide, we defined each of the 5Ps and saw how together they create a rich, explanatory psychological formulation. Unlike a mere diagnosis, a 5Ps formulation captures the person’s story
- what their problems are
- how and why those problems developed;
- what triggers them;
- what keeps them going, and;
- the resources that can help improve the situation.
For both undergraduate and postgraduate students of psychology and counselling, mastering the 5Ps approach is fundamental. It encourages holistic thinking – integrating biological, psychological, and social factors. Plus, it ensures that we can tailor treatment to the individual (Johnstone and Dallos, 2014).
Therapeutic Modalities
We also explored how the model applies across different therapeutic modalities. CBT, psychodynamic, and integrative therapies all benefit from the structured yet flexible nature of 5Ps. Even as they adapt it to their own theories. The 5Ps formulation case study illustrates in practice how a therapist might use the model to make sense of a complex case. As a result, the case study learnings guide a multi-faceted intervention.
The 5Ps model is widely used not only in clinical settings to help clients (and clinicians) make sense of difficulties. It’s also common in teaching and supervision to train new therapists in case conceptualisation skills. Its popularity in services worldwide (from NHS guidelines to psychotherapy handbooks) attests to its value. That said, we noted some limitations and cautions. One must use it thoughtfully and collaboratively to avoid becoming a rote checklist or overwhelming the client.
When used well, the 5Ps formulation is a powerful tool for understanding and improving mental health outcomes. It embodies the principle that to help someone, we must understand them in context: past, present, psychology, environment, and strengths. In conclusion, the 5Ps framework’s comprehensive and structured approach makes it an indispensable part of effective psychological practice, enabling clinicians to craft individualised formulations that lead to more targeted and empathetic care. By appreciating each of the 5 “Ps,” a practitioner can truly “make sense” of a person’s problems and work with them towards positive change (BPS, 2011; Macneil et al., 2012).
References (Harvard style)
- British Psychological Society (2011) Good Practice Guidelines on the use of psychological formulation. Leicester: British Psychological Society.
- Chadwick, P., Williams, C. and MacKenzie, J. (2003) ‘Impact of case formulation in cognitive behaviour therapy for psychosis’, Behaviour Research and Therapy, 41(6), pp. 671–680. DOI: 10.1016/S0005-7967(02)00033-5.
- Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust (2018) Understanding what influences your mental health and wellbeing (Patient Information Leaflet PIC/791/0218). Available at: https://www.cntw.nhs.uk/wp-content/uploads/2018/02/5-Ps-and-formulation-A5.pdf (Accessed 17 March 2025).
- Johnstone, L. and Dallos, R. (2014) Formulation in Psychology and Psychotherapy: Making sense of people’s problems (2nd edn). East Sussex: Routledge.
- Kuyken, W., Padesky, C.A. and Dudley, R. (2009) Collaborative Case Conceptualization: Working effectively with clients in cognitive-behavioural therapy. New York: Guilford Press.
- Macneil, C.A., Hasty, M.K., Conus, P. and Berk, M. (2012) ‘Is diagnosis enough to guide interventions in mental health? Using case formulation in clinical practice’, BMC Medicine, 10, p. 111. DOI: 10.1186/1741-7015-10-111.
- National Institute for Health and Care Excellence (2014) Psychosis and schizophrenia in adults: treatment and management (Clinical Guideline 178). London: NICE.
- Persons, J.B. (1989) Cognitive Therapy in Practice: A case formulation approach. New York: W. W. Norton & Company.
- Peters, S.W. (2020) ‘Case Formulation and Intervention: Application of the Five Ps Framework in Substance Use Counselling’, The Professional Counselor, 10(3), pp. 327–336.
- bMindful Psychology (2023) ‘The power of understanding psychological formulation: A guide for mental health professionals’. Available at: https://www.bmindfulpsychology.co.uk/post/understanding-psychological-formulation (Accessed 17 March 2025).
- Weerasekera, P. (1996) Multiperspective Case Formulation: A step towards treatment integration. Melbourne, FL: Krieger Publishing.
- Comorbidity Guidelines (2023) ‘Case Formulation’, in Guidelines on the management of co-occurring mental health conditions in alcohol and other drug treatment settings. University of Sydney. Available at: https://comorbidityguidelines.org.au/b3-identifying-cooccurring-conditions/case-formulation (Accessed 17 March 2025).
Cite This Work
To export a reference to this article please select a referencing stye below:



